Draft
School Nurse’s Mental Health Toolkit | 1
School Nurse’s
Mental Health
Toolkit
Practical Strategies for Helping Students
Draft
School Nurse’s Mental Health Toolkit | 2
School Nurse’s
Mental Health Toolkit
Practical Strategies for Helping Students
About This Guide ............................................................................................................................................ 3
Mental Health Action Signs for School Nurses ..................................................................................... 4
Coping and Relaxation Strategies ............................................................................................................. 5
Anxiety ................................................................................................................................................................ 7
Panic Attacks ..................................................................................................................................................... 8
School Avoidance ............................................................................................................................................ 9
Depression ....................................................................................................................................................... 10
Depression: Signs of Depression .......................................................................................................... 10
Depression: Strategies to Help...............................................................................................................11
Depression: Cognitive Behavioral Therapy ...................................................................................... 12
Preventing Suicide ........................................................................................................................................ 13
Preventing Suicide: Signs of Ideation ................................................................................................. 14
Preventing Suicide: Strategies and Resources ................................................................................ 15
Self-harm .......................................................................................................................................................... 16
Self-harm: Self-harm vs. Suicidal Behavior........................................................................................ 16
Self-harm: Signs of Self-harm ............................................................................................................... 17
Self-harm: Strategies to Help ................................................................................................................ 18
Anger ................................................................................................................................................................. 19
Anger: Strategies to Help ........................................................................................................................ 19
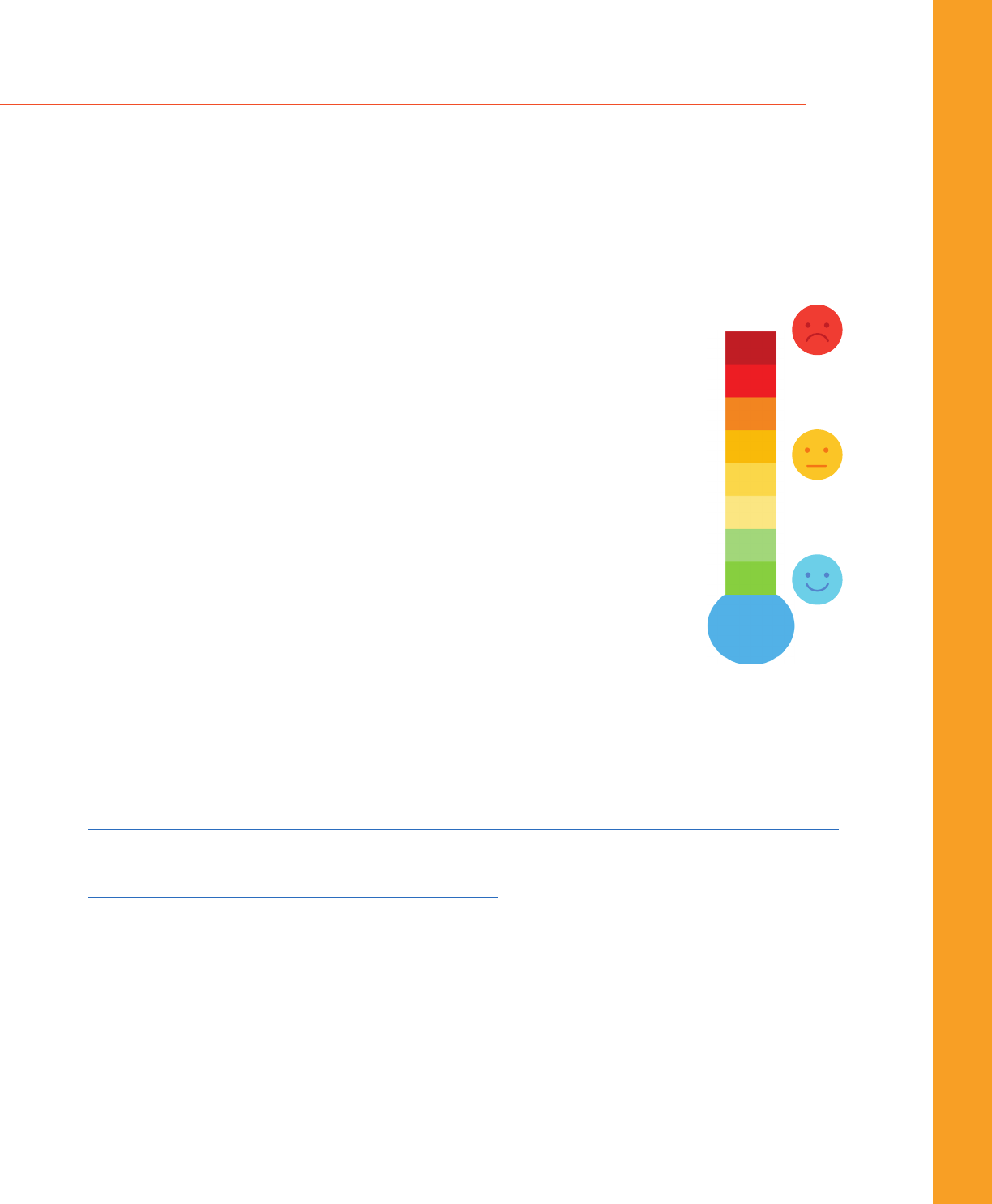
Anger: The Anger Thermometer..........................................................................................................20
Resources ........................................................................................................................................................ 21
Copyright
©
VA-AAP - School Nurse’s Mental Health Toolkit
2024 Edition
Draft
School Nurse’s Mental Health Toolkit | 3
About This Guide
America’s children spend nearly 1,000 hours a year in school.
Who do these kids go to when experiencing mental health distress?
A school nurse.
This toolkit was born from a collaboration in Virginia between school
nurses and pediatricians to learn and partner together to support
children and families with evidence-based tools.
The toolkit is owned by the Virginia Chapter of the American Academy
of Pediatrics. The Resource for Advancing Children’s Health Institute
was instrumental in content writing.
Special thanks to Lisa Hunter Romanelli, PhD.
Virginia schools can order a copy of the toolkit for
their health clinic or download a digital copy from
the VDH School Health webpage:
VDH.Virginia.gov/school-age-health-and-
forms/school-health-guidelines-and-
resources/.
Acknowledgments and Gratitude
Virginia Chapter, American Academy of Pediatrics
School and Mental Health Committees
Jacqueline Cotton, MD, FAAP, project lead, Mental Health
Committee Co-Chair
Leah Rowland, MD, FAAP, project lead, School Health
Committee Co-Chair
Percita Ellis, MD, FAAP, VA-AAP Treasurer, Rural Health Champion
John Farrell, MD, FAAP, School Health Committee Co-Chair
Paula Fergusson, MD, FAAP
R. Emily Gonzalez, PhD, Immigration Health Co-Chair
Amy Harden, MD, FAAP
Paige Perriello, MD, FAAP, Central Virginia VA-AAP Delegate
Kristina Powell, MD, FAAP, VA-AAP President
Bethany Geldmaker, PhD, PNP, VA-AAP grant administrator
Tammy Shackelford, administrative lead,
Virginia Mental Health Access Program
School nurse leadership contributors:
Joanna Pitts, BSN, RN, NCSN, CNOR (lead)
Angela Knupp, BSN, RN
Tammy Miller, BSN, RN, QMHP
Heather “Shea” Pugh, BSN, RN
Children’s Hospital of The King’s Daughters,
graphic design and publication support.
This resource is supported in part by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) as part of an award totaling
$1,167,341 with 20% financed with non-governmental sources. The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by
HRSA, HHS, or the U.S. government. For more information, please visit HRSA.gov.
This resource is being made available by the VA-AAP to the general public and is for informational purposes only. The views expressed in this resource should not necessarily be
construed to be the views or policy of the VA-AAP, or any partners in this work.
The information in this resource is believed to be accurate. However, the VA-AAP does not make any warranty regarding the accuracy or completeness of any information provided. The
information is provided as-is and VA-AAP and its partners expressly disclaim any liability resulting from use of this information. The information in this resource is not, and should not
be relied on as medical, legal, or other professional advice, and readers are encouraged to consult a professional advisor for any such advice.
In addition, this resource is not a substitute for the exercise of one’s independent professional judgment, which shall be exercised in the sole discretion of the individual. No part of this
resource may be reproduced or distributed in any form or by any means without the prior written permission of the VA-AAP.
Download a digital copy and learn more about
the Virginia Chapter of the American Academy
of Pediatrics:
VirginiaPediatrics.org/school-
nurse-toolkit/

Draft
School Nurse’s Mental Health Toolkit | 4
Mental Health Action Signs for School Nurses
Mental Health Action Signs for School Nurses
Despite well-documented levels of emotional and behavioral problems in the nation’s youth, studies
have repeatedly shown that 75% of youth with these problems are not identified and do not receive
needed care.
The REACH Institute offers the “Actions Signs” Project toolkit to help caregivers, educators, and healthcare
professionals identify children at behavioral and emotional risk. If you think that one of your students may
have any of the following signs, take immediate action, collaborate with your school’s mental health team,
and follow your school’s protocol to help your student feel better.
• Feeling very sad or acting withdrawn for more than two weeks.
• Seriously trying to harm or kill themselves, or making plans to do so.
• Sudden overwhelming fear for no reason, sometimes with a racing heart or
fast breathing.
• Involved in many fights, using a weapon, or wanting to badly hurt others.
• Severe out-of-control behavior that can hurt them or others.
• Not eating, throwing up, or using laxatives to make themselves lose weight.
• Intense worries or fears that get in the way of their daily activities.
• Extreme difficulty in concentrating or sitting still that puts them in physical
danger or causes school failure.
• Repeated use of drugs or alcohol.
• Severe mood swings that cause problems in relationships.
• Drastic changes in behavior or personality.
To download the “Actions Signs” Toolkit, scan the code or visit
Flipsnack.com/reachcatie/actionsigns.html.
For more information about youth mental health support,
r
esources, and tools, visit TheReachInstitute.org.
TheReachInstitute.org
Draft
School Nurse’s Mental Health Toolkit | 5
Coping and Relaxation Strategies
Coping and Relaxation Strategies
It is difficult to learn something new when we are anxious, angry, or distracted.
Teach and practice coping skills when everyone is calm.
Breathing Techniques
Belly Breathing
• When we are anxious, we breathe from our chest.
• Belly breathing stimulates the vagus nerve which
activates the relaxation response.
• Exhale longer than inhale for increased effect.
Young Children:
• Lie down so the back is supported by a surface
(couch/floor).
• Place a toy on the belly and watch it rise and fall.
Learn to belly breathe with Elmo:
Visit YouTube.com/watch?v=_mZbzDOpylA
or scan the code.
Older Children:
• Blow on pinwheel for
prolonged exhalation.
• Imagine filling room with a color while exhaling.
Teens:
• Hand on sternum, hand over belly button and focus
on moving hand on abdomen only.
• Counting inhale/exhale pattern: 4 second inhale,
7 seconds exhale.
Belly breathing video demo for
older kids: Visit YouTube.com/
watch?v=OXjlR4mXxSk or scan
the code.
Box Breathing
• Exhale to a count of four.
• Hold with lungs empty for four counts.
• Inhale to a count of four.
• Hold the air in your lungs for a count of four.
• Exhale to a count of 4 and start over.
Learn to box breathe:
Visit YouTube.com/
watch?v=G25IR0c-Hj8 or
scan the code.
Take 5 - Combines breathing and sensory input.
• Trace one hand with the finger on the opposite hand.
• Breathe in deeply as you trace your thumb from base
to tip.
• Breathe out as you trace back to your palm.
• Breathe in as you trace to the tip of your index finger.
• Breathe out as you trace back to your palm.
• Go around your whole hand.
• Can do this under the desk at school.
54321 Coping Strategy
54321 (or 5, 4, 3, 2, 1) is a grounding technique to reduce anxiety or stress. Tell the
student: Identify 5 things you can see, 4 things you can touch, 3 things you can hear, 2 things
you can smell, and 1 thing you can taste.
For video demo, visit Strong4Life.com/en/emotional-wellness/coping/grounding-your-
body-and-mind or scan the code.

Draft
School Nurse’s Mental Health Toolkit | 6
Coping and Relaxation Strategies
Coping and Relaxation Strategies
Muscle Relaxation Technique
Progressive Muscle Relaxation or “Body Scan”
When we are anxious our bodies respond with muscle tension. Progressive muscle relaxation reduces muscle tension
and associated anxiety.
• Tense muscles first – from head to toe – and then release. This allows easier letting go of muscle tension all over the
body.
• This can be done without others noticing, even while in class.
• Squeeze fists as tight as you can (under desk or in pockets) for 10 seconds, then release.
• Squeeze knees together as tight as you can (under desk) for 10 seconds, then release.
For video demo, visit Strong4Life.com/en/emotional-wellness/coping/practicing-progressive-
muscle-relaxation or scan the code.
For video demo for older children, visit YouTube.com/watch?v=8Xp2UzG7UYY or scan the code.
Distraction Strategies
• Choose an item you can see in front of you. Spell it out, forward and then backward.
• Pick a color and name everything you can see that matches that color.
• Hum a song quietly.
• Think about your favorite TV show. Try to remember all the actors’ names and what they were last wearing.
• Focus on one object and think about how you would change each aspect of its design.
• Choose a category (what you see around you, animals, countries, people, food, etc.) and try to name one item for
each letter of the alphabet.
Ways to distract yourself at home:
• Listening to music.
• Watching TV.
• Reading.
• Drawing.
Door Method Relaxation Technique*
This technique can be helpful for falling asleep, staying calm, and
reducing distractions.
• Picture four doors, all hiding a place or something that brings joy.
• Pick a door you want to go in and walk in. What do you see there?
Look around and describe all that you experience - sights, sounds,
and smells.
*Door Method by Tamar Chansky from “Freeing Your Child from Anxiety”, 2004.
The
Beach
Grandma’s
House
The
Park or
Playground
Kittens
Draft
School Nurse’s Mental Health Toolkit | 7
Anxiety
Anxiety
Everyone experiences anxiety. Anxiety is a common emotion and can be helpful or harmful.
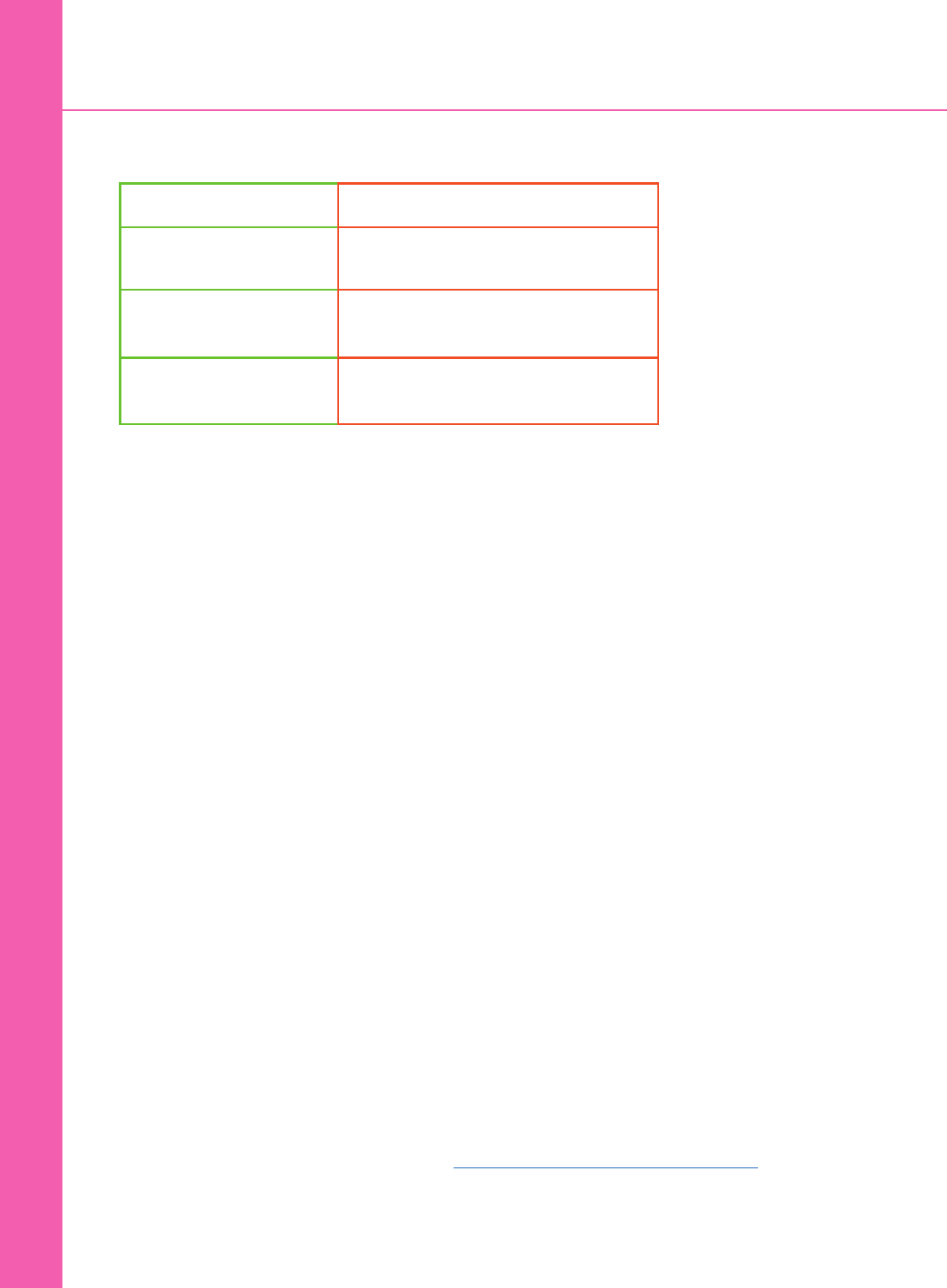
Anxiety is helpful: Anxiety is harmful:
To protect us when there is
a real threat.
When we see threats everywhere.
To alert us to a stressful
situation.
When we overestimate threat so that
most situations are stressful.
To help us face new
challenges.
When we avoid daily activities and new
challenges.
Past or present trauma can provoke
anxiety symptoms.
Students with severe anxiety can
have self harming behaviors or
suicidal thoughts.
Signs of Anxiety
Academic signs:
• Frequent trips to the nurse.
• Leaving school early or arriving late.
• Skipping school activities (e.g., gym, lunch,
or recess).
• Excessive absenteeism.
• Sleeping in class.
Student might report:
• Physical complaints (stomach aches, headaches,
chest pain, racing heart, trouble breathing, feeling
dizzy).
• Excessive worry or fears.
• Trouble concentrating.
• Feeling afraid as if something awful might happen.
• Trouble sleeping.
Signs others might see:
• Restlessness.
• Irritability or acting out.
• Using marijuana or other drugs to ease distress.
• Change in participation in normal activities.
• Not wanting to engage with friends or activities.
Immediate Strategies
Listen and support.
Let the student know that you hear how they are feeling
and that you are there to help.
Communication Tips
• Validate the student’s feelings: “It sounds like you’re
worried about ...That must be very hard.” Avoid saying
“Everything is fine,” “Don’t worry,” or “That’s not a big
deal.”
• Check your feelings. Be calm, so you can calm the
student.
• Gather information without judgment. Be curious.
• Do you know why you’re feeling worried?
• What challenges are you having at home or
school?
• How are your worries affecting your sleep and
concentration?
• How do your worries make it hard to do what
you normally do?
• How often does this happen?
• Explain anxiety. Let the student know that everyone
gets anxious. Anxiety is helpful when there is a real
danger or true alarm. Sometimes, we get a false alarm
and overestimate the threat.
Review the Cognitive Behavior Triangle - Visit the Depression section in this guide.
Students with severe anxiety can be treated with therapy or medication or both. Changing one piece of the triangle
(e.g., improving self-talk/thoughts) affects feelings and behavior. For example, changing a thought from “I’m going
to fail this test” to “I studied and I’ll do my best” can decrease anxiety (feeling) and improve concentration (behavior).
Changing behavior (deep breathing exercises) can improve anxiety (feeling) and help thoughts become more positive.
Draft
School Nurse’s Mental Health Toolkit | 8
Panic Attacks
Panic Attacks
A panic attack is a period of intense fear or discomfort during which at least four symptoms of anxiety
develop quickly and usually reach a peak within 10-20 minutes.
Students may experience panic attacks out of the blue or in response to a feared object or situation (e.g., a spider,
taking a test, giving a presentation).
Signs/Symptoms
During a panic attack, a student will experience at least four of the following symptoms intensely:
• Pounding heart or accelerated heart rate
• Sweating
• Trembling or shaking
• Shortness of breath
• Feelings of choking
• Chest pain
• Nausea or stomach pain
• Dizziness or lightheaded
• Numbness or tingling sensations
• Chills or hot flashes
• Fear of losing control or going crazy
• Fear of dying
• Feeling detached from reality
Strategies
Panic attacks are scary to experience and witness. You can help a student having a panic attack by:
Staying calm. Students are overwhelmed during a panic attack and may think they are going to die. By
staying calm and speaking to the student in a soothing voice, you can help them to relax more quickly.
Providing reassurance. Let the student know that they are experiencing a panic attack, it is scary, but
harmless and will pass. They are going to be fine. Reassure them that the symptoms will usually stop in
10 -20 minutes and you can help them feel better.
Showing the student how to slow down their breathing. A lot of the symptoms of panic are triggered
by over breathing (hyperventilating). Encourage the student to try to slow down their breathing by taking
slow, quiet, belly breaths in through their nose with their mouth closed and then out through their mouth.
The greater the panic, the more time it will take for a student to be able to slow down their breathing.
Helping the student feel more grounded. A variety of mental and physical grounding techniques can
help a student shift their focus away from the symptoms of panic. For example, try the 54321 technique
or apply cold water or an ice pack to the face and hands.
Gathering information. Once the student is calm, you can be curious and non-judgmental to find out if
this is happening frequently, and connect them with resources via your school protocols.
988
SUICIDE
& CRISIS
LIFELINE
Help them connect.
Always follow your school’s crisis protocols.
Call or text 24/7.
988 for the Suicide & Crisis Lifeline.
Draft
School Nurse’s Mental Health Toolkit | 9
School Avoidance
School Avoidance
School avoidance is the regular refusal to attend school or maintain consistent attendance. This can lead
to chronic absenteeism, missing 18 days or more of school within an academic year. The sooner school avoidance is
recognized, the better: not attending school is an emergency. Multiple factors contribute to school avoidance.
External factors:
• Bullying from a student or adult in
the building.
• Family violence, trauma, or
disruption.
• Family illness leading to separation
anxiety.
• Poverty, lack of access to resources,
need to work to support the family.
• Racism or LGBTQ+ discrimination.
• Natural disasters, violence in the
community.
Student factors:
• Mental health conditions
(depression, anxiety).
• Personal medical challenges
(e.g., constipation causing
student to avoid using the
bathroom at school).
• Chronic or acute medical
illness (e.g., diabetes,
concussion).
What others might see:
• Refusal to participate in class
activities (recess, PE, etc).
• Temper tantrums or outbursts,
crying, especially upon arrival to
school.
• Improvement on weekends or
breaks.
• Chronic tardiness or early
departures.
• Missing class, presentations,
or tests.
• Frequent clinic visits.
Strategies
Unmet needs contribute to school avoidance.
Develop a communication process and team within the school so nurses are made aware of students who are
missing school but may not be coming to clinic.
Check in with the student:
Ask open ended questions, starting with easy ones.
• Be curious and supportive – “You have been missed
lately! How are you?”
• Have you been sick? How have you been feeling?
• What do you like (or dislike) about school these days?
• Can you tell me about your friends? Are you being
bullied by anyone?
• Has anything scary happened at school?
• How is everything going at home? What kind of
changes are happening?
• Is there anything specific (classes or stressful
situations) that keeps you from school?
• If chronically tardy, say: “I see you are often late in
the morning. What do your mornings look like? How
is everything at home? How can I help?”
Provide personalized early outreach to families.
The longer a child misses school, the harder it is to
return. Connect with an open mind:
• “I am calling to see how we can support you and
[student] in order for [him/her] to be in school
regularly. Are there any specific reasons that your
child has been absent?”
• If chronically tardy, ask: “Are there ways we can
help your child arrive on time?”
• Recognize that stepwise approaches can be
helpful. Consider a 504 plan for gradual re-entry
to school.
• Connect families to local resources.
See Bridge2ResourcesVA.org.
• Encourage a visit to their medical provider.
Encourage intra-school connectedness. A counselor, trusted teacher or coach, extra curricular activities,
and clubs help students’ motivation to attend. Who can be on the support “team” for the student?
Recognize when students need a 504 plan or IEP for unmet medical or educational needs.
Draft
School Nurse’s Mental Health Toolkit | 10
Depression
Depression
Depression is a mood disorder that affects how we think, feel, and act.
It can be described as overwhelming sadness that persists, interfering with everyday life.
For at least two weeks, students may
experience:
• Excessive sadness (may see irritability or
anger).
• Loss of interest in activities.
• Change in appetite, may see weight loss
or gain.
• Sleeping too much or too little.
• Feeling restless or hard to get moving.
• Fatigue and trouble concentrating.
• Feelings of guilt or low self-esteem.
• Thoughts of death or dying.
Did you know?
• Risk factors for depression include a family history of depression, stress, co-existing mental health disorders, and
chronic medical illnesses.
• Younger students present more often with physical complaints such as chronic abdominal pain and recurrent
headache.
• Black youth are less likely to seek help and less likely to remain in counseling.
• LGBTQ+ youth are SIX times more likely to be depressed.
ASK
Depression can be associated
with suicidal thoughts, plans, or
attempts. One caring adult can
save a life! There is NO EVIDENCE
that asking about suicide increases
its risk. Don’t wait to take action!
Quick Strategies
• Approach with curiosity,
not judgment.
•
A
sk open-ended
questions.
•
O
ffer hope.
Signs
Thoughts:
• Circular negative thinking: “I’m not good
enough, nothing is going to get better.”
• Emptiness or numbness. A lack of joy.
• Suicidal thoughts: “It’s not worth it to go on.”
Actions:
• Dropping out of activities.
• Not spending time with family or friends.
• Staying in their room at home.
• Self-harm.
Behaviors noticeable to others:
• Distancing, withdrawal, acting out.
• Change in friend groups or isolation.
• Concerning social media activity.
• Decline in hygiene or no longer caring about appearance.
• Changes in eating habits (e.g., not eating lunch).
Academic changes:
• Skipping classes.
• Acting out in class toward teachers or peers.
• Falling asleep in class.
• Decline in academic performance.
• Difficulties concentrating.
Draft
School Nurse’s Mental Health Toolkit | 11
Depression
Depression
Strategies
School nurses can do a lot to help
depressed students.
Approach with curiosity, not judgment.
Ask open-ended questions.
“I have seen changes that make me wonder about you.
Are you doing OK? How are you feeling?”
“I see you are really struggling. Is there anything you
would like to talk about?”
“I have heard others say I just want the pain to go away –
how about you?”
Offer hope. Share information about depression.
If you suspect a student may be depressed, you can
tell the student:
Depression is common but not normal.
Depression changes how we think, feel, and act.
Depression can cause physical changes.
Depression is treatable. Therapy, learning new skills,
and sometimes medication can help depression.
Encourage the student to share how they are
feeling with people they trust.
Depressed students need support, but may not let
people know how they are feeling. Encourage students
to let trusted friends, caregivers, teachers, and medical
providers know how they are feeling.
Notify appropriate school staff if you’re concerned
about the severity of the student’s depression or
suspect the student is suicidal.
Know your school’s protocol and crisis team before a
crisis, and follow up after referral.
Communicate with caregivers and providers.
Encourage families to contact medical providers
about your concerns so they can collaborate to make a
treatment plan.
Visit Bridge2ResourcesVA.org or scan
the code to help families identify local
mental health resources.
Cognitive Behavioral Therapy
Cognitive behavioral therapy shows the connection between feelings, thoughts, and behaviors. If we can recognize
these interactions, we can figure out ways to feel better when we are experiencing distress.
• Teach calming methods to relax the mind and body. See Coping and Relaxation Techniques section in this guide for
more information.
• Change your behavior or environment. Go outside, find a friend, listen to music, draw, or move the body (shoot
baskets, kick a soccer ball, or walk).
• Create a toolbox. Help them write down strategies that work. What can the student do the next time they feel sad?
• Explore ways to create healthy routines. Getting adequate sleep and nutrition, reducing screen time or social media
use, exercise, or increasing free time and friend time matters to well-being.
• Follow school protocols for mental health referrals when depression is moderate or severe, and/or has been occurring
for longer than two weeks.
Draft
School Nurse’s Mental Health Toolkit | 12
Depression
Depression
Helpful cognitive behavioral strategies for depression are gifts that a nurse can give students in the moment.
They include:
Thoughts – Depression is associated with negative thoughts and core beliefs such as, I am unlovable, I am
worthless, and I am helpless. Changing thoughts can help change feelings and behaviors (see CBT triangle). Some
questions that can help students “put their negative thoughts on trial” are:
• “Is this thought helping or hurting me?”
• “What is the evidence for and against the thought?”
• “Is there a more helpful and realistic thought?”
• “What would my friends say?”
Feelings – Encourage students to cope with feelings of immediate sadness by doing something that is fun and
distracting, soothing and relaxing, or that expends energy.
• Increase pleasurable activities.
• Teach the student: depression may tell you to stay home by yourself, but put yourself into positive situations
even if you don’t feel like it and see what happens.
• What does the student like to do? Help the student identify and schedule fun: exercise, art, music, writing,
group or family activities.
Behavior – Unpleasant situations, interpersonal conflicts, and stressors can contribute to depression. If these things
are under the student’s control, encourage problem solving. Key steps for problem solving are:
1. Problem Identification (what is the problem?)
2. Identify Choices (what choices can I make?)
3. Consequences (what might happen if I make that choice?)
4. Choose a Solution (make a decision and go!)
Thoughts
FeelingsBehavior
Draft
School Nurse’s Mental Health Toolkit | 13
Preventing Suicide: How to Help
988
SUICIDE
& CRISIS
LIFELINE
One caring person can save a life…
You are that person.
Prevention of suicide involves
identifying students who have:
• Thoughts of death or hurting
themselves.
• A history of prior attempts.
• A specific plan.
• A family history of suicide.
Risk factors include:
• Bullying.
• Chronic illness.
• Depression or other mental health
disorders.
• Inability to obtain care for mental
health.
• Societal pressures (racism, poverty, or
trauma).
• Stigma and cultural barriers.
• Substance abuse.
• Access to lethal means.
Firearms are
used in more
than 50% of
suicides.
Help them connect.
Always follow your school’s crisis protocols.
Call or text 24/7.
988 for the Suicide & Crisis Lifeline.
To text 988 in Spanish, type “Ayuda” to connect with a Spanish-speaking counselor. For people who speak
other languages, call 988 for translation in 240+ languages. This is available 24/7 through voice calling only.
ASK
There is NO EVIDENCE
that asking about
suicide increases its risk.
Quick Strategies
• Approach with
curiosity, not
judgment.
• Ask open-ended
questions.
• Offer hope.
Preventing Suicide: How to Help
Draft
School Nurse’s Mental Health Toolkit | 14
Suicide rates are higher for:
• Black youth - Rates of suicide for Black youth have risen faster than in any other racial/ethnic group in the past
two decades.
• LGBTQ+ youth.
• Native Americans and Alaska natives.
• Those with disabilities (due to difficulties in communicating suicidal thoughts).
• Residents of rural areas.
Signs
Noticeable Behaviors
• Withdrawal or reports of severe pain.
• Extreme mood swings, including irritability or anger.
• Giving away prized possessions.
Actions
• Talking about wanting to die.
• Making or researching a plan to die.
• New or increased substance use.
Preventing Suicide: How to Help
Preventing Suicide: How to Help
Suicidal Ideation in Students
In 2021, approximately 3% of
all students reported making
a suicide attempt that
required treatment.
In 2021, suicide was the second
leading cause of death for youth
ages 10-14 and ages 20-34.
In 2017, nearly 1 in 5 students
had thoughts of suicide. This
increased to 1 in 4 during
the pandemic.
Thoughts
• Frequent thoughts about death or dying.
• “I don’t want to live.”
• “Everyone would be better off without me.”
• “It’s all my fault.”
Academic Signs
• Withdrawal from activities or declining grades.
• Chronic absences.
• Dramatic change from prior performance.
For additional resources for mental health conditions associated with suicidal ideation for
additional resources for mental health conditions associated with suicidal ideation, scan
the code or visit TheREACHinstitute.org/help-for-families/helpful-resources/. For additional
resources about suicide prevention, visit the American Foundation for Suicide Prevention
at AFSP.org.
Draft
School Nurse’s Mental Health Toolkit | 15
Preventing Suicide: How to Help
Preventing Suicide: How to Help
988
SUICIDE
& CRISIS
LIFELINE
Strategies
Approach with curiosity, not judgment.
“This is a horrible way to feel, but there is help and hope for feeling better.”
“Thank you for sharing these thoughts. I am here with you.”
Ask open-ended questions.
“Sometimes kids feel so low that they wish they were never born. How about you?”
“Sometimes when people feel this bad, they wish they were dead or not here anymore.
Tell me about you…”
“Have you ever done something to hurt yourself or tried to kill yourself?”
Offer hope.
“These feelings are treatable. Therapy, learning new skills, and sometimes medication can help.”
“You are not alone. Many kids have experienced the same feelings and have gotten better.”
Additional Resources
Download the Ask Suicide-Screening Questions toolkit at NIH.NIMH.gov. These screening questions can be
completed with a student in one minute to determine if they need emergent care.
Visit SuicideSafetyPlan.com for the The Stanley Brown Safety Plan (also available for
download in the Apple App Store or scan the code).
Safety planning is an essential part of treatment. For more information, visit AFSP.org.
Having a safety plan that addresses the following is an essential component of a student’s recovery:
• Recognize what puts a student at risk.
• Find coping strategies that do not rely on the presence of others.
• Engage with people and go to places that help distract students away from their problems.
• Reach out to family or friends that can help students in a crisis.
• Keep the student’s environment safe.
• Consider sharing the home safety checklist with families: AACAP.org/AACAP/AACAP/Families_and_Youth/
Facts_for_Families/FFF-Guide/suicide-safety-130.aspx.
Keep the student safe with you while you contact school resources.
Connect and communicate with school staff, caregivers, and pediatric clinicians. Know your school’s protocol and
crisis team before a crisis, and follow up after referral.
Help them connect.
Always follow your school’s crisis protocols.
Call or text 24/7.
988 for the Suicide & Crisis Lifeline.
To text 988 in Spanish, type “Ayuda” to connect with a Spanish-speaking counselor. For people who speak other
languages, call 988 for translation in 240+ languages. This is available 24/7 through voice calling only.
Draft
School Nurse’s Mental Health Toolkit | 16
Self-harm
Self-harm
Self-harm (non-suicidal self-injury) occurs when a person
hurts oneself on purpose.
ASK
Suicidal thoughts can
be present in a person
who self-harms (but
self-harm does not
automatically mean a
person wants to die).
• Behavior might be a momentary escape
from intense distress such as loneliness,
sadness, fear, or shame.
• Sometimes it is hard to stop because it
helps them feel better.
• Self-harm can be a way to take control
when everything else is out of control
(family conflict, bullying, or trauma).
Did you know?
• Self-harm is a cry for help.
• Kids and teens with mental health
conditions are at the highest risk for
self-harm. These include:
• Depression.
• Substance abuse.
• Sexual abuse.
• Severe abuse or abuse by a
family member.
• Anxiety disorders.
• Eating disorders.
• PTSD.
• Borderline personality disorder.
• Average onset for self-harm is 15 years
old but females are more likely to be
younger.
• Of people who self-harm, 25% only
have one episode.
• The majority of people who self-harm
stop after a period of five years.
• Severity of self-harm can range
from superficial wounds to lasting
disfigurement.
Self-harm might include:
• Cutting.
• Burning.
• Hair pulling.
• Skin-picking or biting.
• Hitting or punching self with intent to
cause harm.
• Risky behaviors (trying to get hurt on
purpose).
Draft
School Nurse’s Mental Health Toolkit | 17
Self-harm
Self-harm
WHY?
What are some
possible reasons
a person would
s
elf-harm?
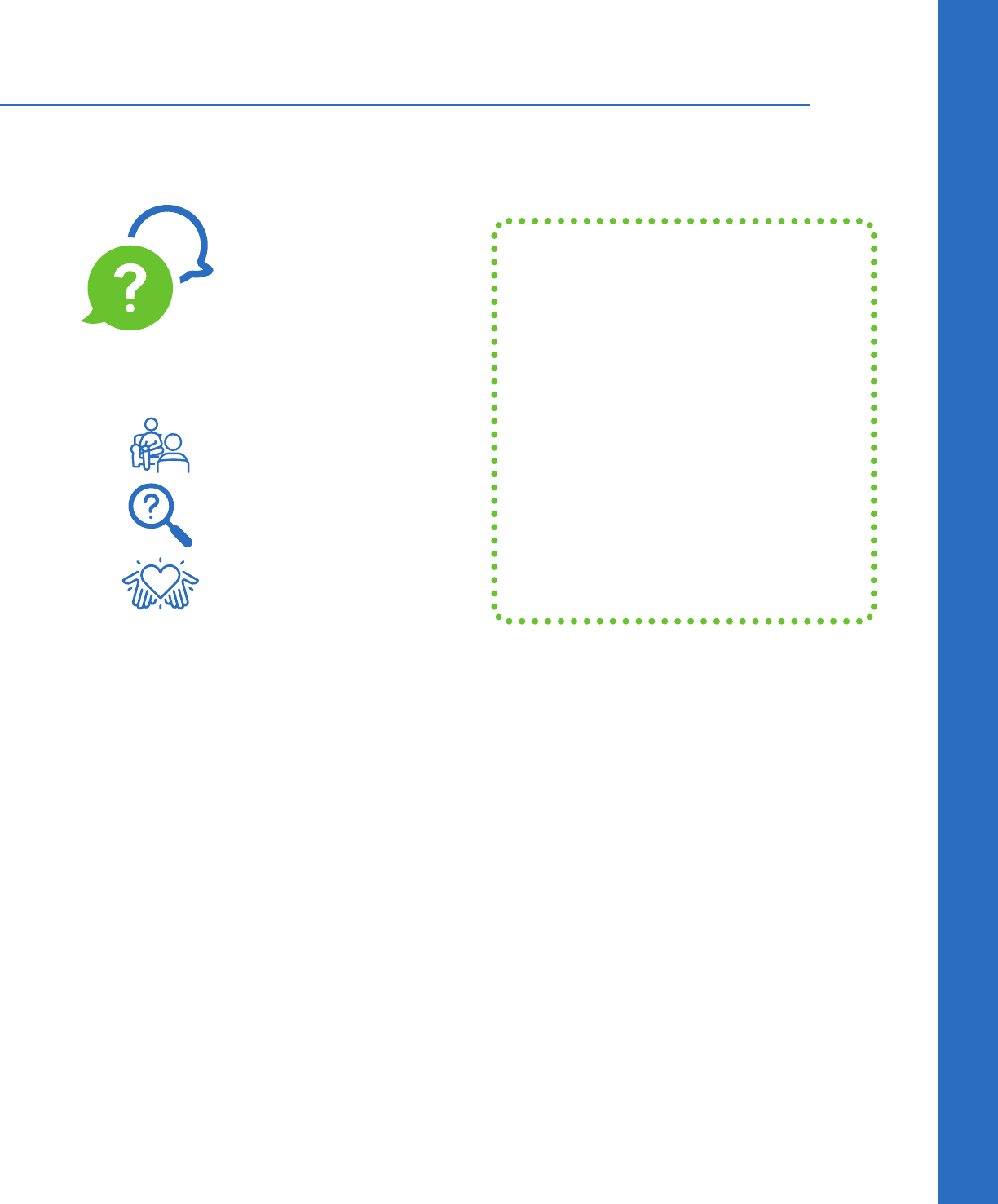
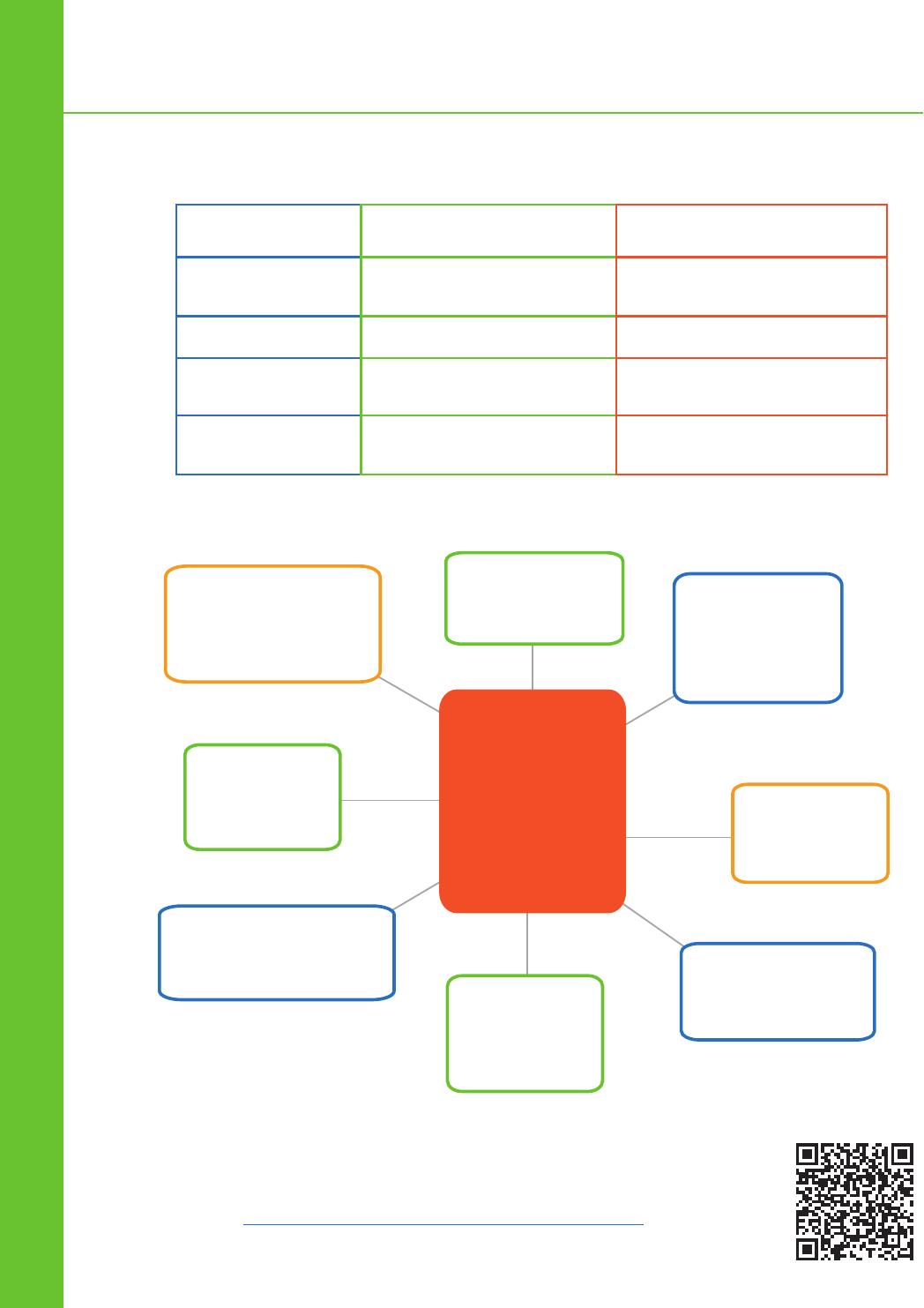
Self-harm vs. Suicidal Behavior
Self-harm Suicidal Behavior
Intent
To get immediate relief from
negative emotions
To die in order to permanently
escape pain
Repetition
More frequent Less frequent
Lethality
Less lethal means but potential
for fatality
Tends to involve more lethal
means
Psychological
Consequences
Often used to relieve
psychological pain
Often aggravates psychological
pain
To have an
energy rush and
feel good.
To feel in
control of body
or mind.
To relieve
stress or
pressure.
To feel
something.
Sometimes there is
no distinct reason.
To cope
with a history
of trauma.
To cope with anxiety
or negative feelings.
To distract
o
r purify
th
emselves.
WHY? self-harm graphic data is provided by the Cornell Research Program on Self-injury
and Prevention. For more information on self-injury, intervention, and treatment, scan
the code or visit SelfInjury.bctr.cornell.edu/perch/resources/siinfo-2.pdf.
Draft
School Nurse’s Mental Health Toolkit | 18
Self-harm
Self-harm
Signs
What you might see:
• Scars often in patterns (hands, arms, thighs, stomach).
• Fresh cuts or wounds.
• Wearing long sleeves or long pants to hide injury even in hot weather.
What you might hear from the student:
• Frequent reports of accidental injury or risky behavior.
• Problems in relationships with family or peers.
• Mood changes that are impulsive or intense.
• Signs of depression or anxiety.
• Abuse of alcohol, marijuana, or drugs.
• Asking for bandages but not showing wounds.
What peers or family might see:
• Spending time on websites, message boards, or social media devoted to self-harm.
• Exchanging texts devoted to self-injury topics.
• Exchanging photos of self-harm wounds.
• Talking about self-harming behaviors in general or about self-harming thoughts.
Strategies
Approach with curiosity, not judgment.
Ask open-ended questions.
“Sometimes, when some kids are stressed, they hurt themselves on purpose.
Have you ever hurt yourself on purpose without intending to die?”
“I’ve seen those scars on your arms and I think you might be hurting yourself.
If you are, I want you to know that you can talk to me about it.”
Asking questions does not make the student engage in self-injuring behavior.
Offer hope.
“You are not alone. Many students have experienced the same feelings and have gotten better.”
“These feelings are treatable, and you can develop safer ways to deal with negative feelings than
hurting yourself.”
Keep the student safe with you while you contact school resources.
Connect and communicate with school staff, caregivers, and pediatric clinicians. Know your school’s protocol
and crisis team before a crisis, and follow up after referral.
Draft
School Nurse’s Mental Health Toolkit | 19
We all experience anger.
Anger is a secondary emotion.
What is underneath?
Anger occurs when we feel attacked,
threatened, afraid, disrespected, or
humiliated.
Outbursts can be a sign of anxiety, depression,
trauma, stress, or poor emotional regulation.
Underlying mental health conditions or
challenging life situations can lead to anger.
Students often need support to learn how to
manage their anger and minimize the risk of
aggressive behavior.
Strategies
SAFETY FIRST: If a student is displaying anger AND aggressive behavior that is risky to the student and
others, follow your school’s crisis intervention plan.
Manage your own emotions. Angry students may trigger feelings of anxiety and anger in you. Before you can help,
you must manage your own feelings and remain calm. Raising your voice will escalate the student’s emotion.
Be aware of your own body language and position. Take a non-threatening stance and project calm.
Minimize demands on the student. When a student is angry, set aside demands (“lower your voice, sit down, show me
your pass”) until the student calms. Placing demands on an angry student is likely to increase their anger.
Offer supportive comments and choices. In the heat of an angry moment, students need to feel supported and to
calm down before they can engage in any problem solving:
• Say “I can see you’re really upset. Would you like to talk or take a few minutes to relax in my office?” This shows the
student that you understand and allows them to decide how you can help.
• Give choices to promote calm in the moment. Offer a quiet corner, reading, drawing, coloring materials, belly
breathing, 54321, music, or stress balls and other fidget items. Go for a walk with them.
• Listen without judgment. Students may need to vent without interruption, or talk through their feelings with you or
someone they trust. You don’t have to solve the problem in order to help.
Teach these ways to understand anger:
Mindfulness
Mindfulness helps us understand and deal
with distress and to purposefully observe one’s
own thoughts and feelings with kindness, not
judgment.
Encourage students to slow down, accept their
emotions, and focus on breathing.
Once the student is calm, explain that everyone
experiences anger. It can hurt us and others if we
don’t recognize it and know what to do.
Picture anger as a wave. Be mindful of when you’re at the top
of the wave, then ride the wave, waiting until anger levels fall.
The tension and “adrenaline” during peak anger is temporary
and students can learn to wait for it to pass. The wave
visualization can help the student manage their anger.
Picture anger like an iceberg. The anger shows, but there are
other emotions underneath. Ask: “Is your anger hiding another
feeling?” (e.g., sadness, worry, etc.)
Anger
Anger
Draft
School Nurse’s Mental Health Toolkit | 20
Anger
Anger
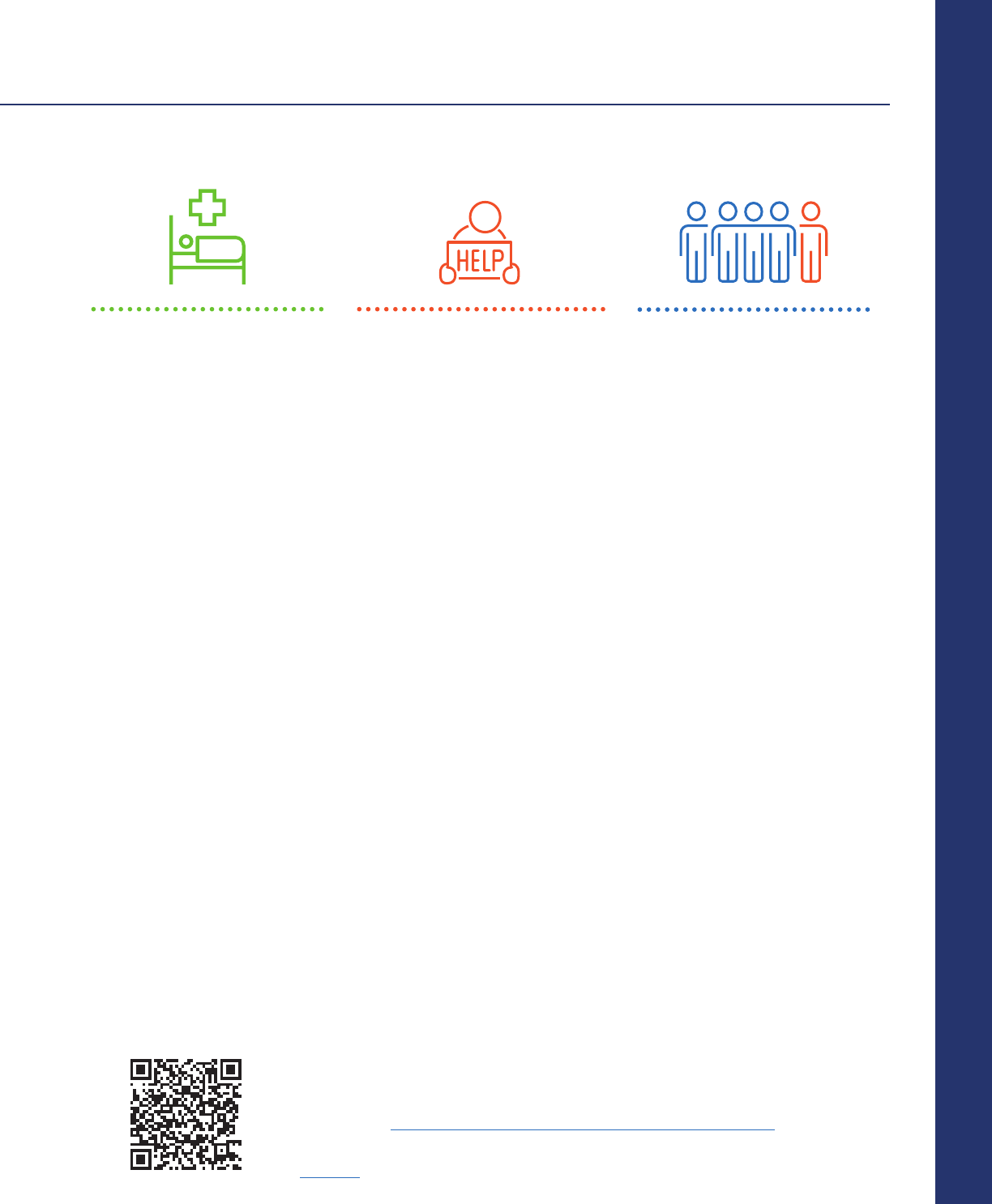
The Anger Thermometer
Teaching students about how to measure their anger using an anger thermometer can help them manage anger.
Teaching The Anger Thermometer to Students
Show the student how the levels on the thermometer correspond to their emotions and bodily feelings.
How does the student feel and behave:
1. When they are most angry?
2. When they are in the middle or upset?
3. When they are peaceful?
4. When students learn about how anger feels in their body
and mind, relating to the anger thermometer, students can:
• Put words to their feelings.
• Start to employ different coping strategies.
• Identify when they need to calm down before acting.
10. I explode
9. Out of control
8. Furious
7. Very angry
6. Angry
5. Upset
4. Somewhat cranky
3. Restless
2. Still and calm
1. Totally at peace
Anger Management Quick Tips
Adapted with permission from Bunge et al. (2017).
Encourage students to practice using these strategies before their anger temperature rises to a high level.
Relaxation strategies – take a time out, belly breathing, applying cold over upper part of face with ice pack,
tensing and releasing muscles.
Mindfulness strategies – 54321, focusing on all your senses.
Distraction strategies – focusing attention on something else (e.g., favorite song, reading, coloring, exercising, object
in the room).
Changing thoughts – When we can identify unhelpful thoughts that fuel anger, and change them to helpful
thoughts, our anger can lessen. For example:
• They don’t control me. I’m not taking the bait.
• I can stay calm.
• As long as I keep my cool, I’m in control
.
Draft
School Nurse’s Mental Health Toolkit | 21
Resources
Resources
Always call 911 for any emergency or when safety is at risk.
Suicide
The Steve Fund Crisis Text Line: Text HOME to 741741; and text STEVE to 741741 if a young person of color, for a trained crisis counselor, 24/7.
Suicide Hotline:
1 (800) 273-TALK (8255)
Self-harm
Young Minds UK - Self-Help Guide for Teens Who Self-Harm video
YoungMinds.org.uk/young-person/my-feelings/self-harm/#Whatisselfharm
Nip in the Bud - Learning about Children’s Mental Health through Film self-harm resources and videos
Nipinthebud.org/films-parents-category/self-harm/
The Cornell Research Program on Self-injury and Recovery -
The Non-Suicidal Self-injury Assessment Tool -
Selfinjury.bctr.cornell.edu/perch/resources/fnssi.pdf
Developing and Implementing School Protocol for Non-Suicidal Self-injury in School -
Selfinjury.bctr.cornell.edu/documents/schools.pdf
Educators and Self-injury: Manual for understanding and aiding students who self-injure.
EducatorsandSelfinjury.com/self%20injury-protocol/
Depression
MindDoc: Mental Health Support- App Download CBT Mood tracker, journal, symptom screener for anxiety and depression. Can also be used
with sleep disorders, eating disorders, postpartum depression, and various phobias. 10-question assessment directs user to learning modules.
Ages 12+, free with in-app purchases, available for download in the Apple App Store and the Google Play Store.
Self Help Toons -
SelfHelpToons.com Free animated self-help video courses about therapy and mental health.
Boston’s Children’s Hospital Guided Self-Management Tools for Depression in Children Ages 6-12. Scan the code.
The ABCs of CBT: Thoughts, Feelings, and Behavior Triangle Cognitive behavior therapy video.
YouTube.com/watch?v=Stw9P38ePVI
Anger
They Are The Future: Anger Thermometer Worksheet Pack - Free printable anger thermometer and parent guide
Theyarethefuture.co.uk/wp-content/uploads/2023/03/Free-Printable-Anger-Thermometer-Worksheets.pdf
Cookie Monster Practices Self Regulation by Life Kit Parenting and NPR - Video about practicing self control.
YouTube.com/watch?v=j0YDE8_jsHk
Mental Health Center for Kids: Videos on anger management for kids.
Anger Iceberg Activity - YouTube.com/watch?v=AQIQCOY_Im0
Strategies to Calm Down When Your Temper Rises - YouTube.com/watch?v=lxxpDF45TPA
Sesame Workshop Handling Angry Feelings for Kids Anger management video. SesameWorkshop.org/resources/handling-angry-feelings/
Panic/Anxiety
Rootd: Panic Attacks & Anxiety - App Download Panic Attack and Anxiety Relief tool. Free with in-app purchases.
Available for download in the Apple App Store and the Google Play Store.
K
ids Helpline Brain Basics: Panic attack informational video series for kids.
YouTube.com/watch?v=geoiskj4aUE
Mindshift CBT- Anxiety Relief App Download Anxiety and stress tools that include fear ladders, goal-setting tool; CBT to reduce worry, stress,
panic. From Anxiety Canada. Ages 12+, available for free download in the Apple App Store and the Google Play Store.
Anxiety Canada -
AnxietyCanada.com
Free downloadable resources and tools for anxiety.
Fight Flight Freeze - A Guide to Anxiety for Kids video: Scan the code.
Fight Flight Freeze - A Guide to Anxiety for Teens video: Scan the code.
Boston Children’s Hospital -
Managing Anxiety in Childhood and Adolescence: Information and resource guide for parents and caregivers.
ChildrensHospital.org/sites/default/files/2023-04/bchnp-managing-anxiety-booklet.pdf
Child Mind Institute - ChildMind.org/topics/anxiety/ Resources for caregivers to support kids with anxiety.
988
SUICIDE
& CRISIS
LIFELINE
Help them connect.
Always follow your school’s crisis protocols.
Call or text 24/7.
988 for the Suicide & Crisis Lifeline.
To text 988 in Spanish, type “Ayuda” to connect with a Spanish-speaking counselor. For people who speak other languages,
call 988 for translation in 240+ languages. This is available 24/7 through voice calling only.
Draft
School Nurse’s Mental Health Toolkit | 22
Resources
Resources
LGBTQ+ Support
The Trevor Project
24/7, 365 crisis support for members of the LGBTQ+ community. Talk, text, or chat.
1 (866) 488-7386
TheTrevorProject.org
Trans Lifeline Peer Support US:
1 (877) 565-8860
The GLBT National Youth Talkline (youth serving youth – age 25):
1 (800) 246-7743
Trauma
Child Mind Institute Video and Guide: Helping Children Cope After a Traumatic Event: Scan the code.
The National Child Traumatic Stress Network - Free resources on child trauma, trauma learning modules,
and tools to develop the systems to gain knowledge, to build practices, and to have the skills to support a trauma-sensitive school.
NCTSN.org/
School Avoidance
School Avoidance Alliance: School Avoidance 101 for Parents - Guide to helping kids get back in school.
SchoolAvoidance.org/school%20avoidance-101/
Rogers Behavioral Health School Avoidance and Refusal: What clinicians need to know. YouTube.com/watch?v=Rw-aBeSygm8
Space Treatment Overcoming Entrenched School Refusal: A six-point plan helping parents for getting school-refusing children back in school.
YouTube.com/watch?v=J4x4NW1S_po
Center on Positive Behavioral Interventions and Supports:
Improving Attendance and Reducing Chronic Absenteeism - Scan code for clinician guide.
School Refusal Assessment and Intervention - Scan the code for clinician guide.
Coping and Relaxation
Mental Health Center for Kids: Grounding Exercises For Anxiety And Other Big Emotions video
YouTube.com/watch?v=5YtnpPPnqaY
Virtual Calming Room: Resource site for students, families, and staff to find tools and strategies for
managing emotions and feelings.
CalmingRoom.scusd.edu/home
The Virginia Tiered Systems of Supports
Led by the Virginia Department of Education to support divisions with implementing and
sustaining a multi-tiered system of supports. A systemic, data-driven approach that allows
divisions and schools to provide evidence-based practices and interventions to meet the
needs of their students. VTSSRIC.vcu.edu/
Other Mental Health Resources
Bridge 2 Resources
Access free or low-cost resources for housing, food, or healthcare in your community. Scan the code.
Bridge2ResourcesVA.org
National Center for School Mental Health (NCSMH): Mental health webinars from the University of Maryland School of Medicine
SchoolMentalHealth.org/webinars/
Stigma-Free Mental Health Student Mental Health Toolkit: Resources for teachers and counselors to help students ages 7-11 and 12-22
improve their mental wellness and combat stigma.
StigmaFreeMentalHealth.com/programs/school-program/student-mental-health-toolkit/
National Association of School Psychologists: The professional home for school psychologists. Site offers standard practice guidelines and a
variety of school-based mental health resources. NASPonline.org/
Substance Abuse and Mental Health Services Administration - Ready, Set, Go, Review: Screening for Behavioral Health Risk in Schools
SAMHSA.gov/sites/default/files/ready-set-go-review-mh-screening-schools.pdf
Mental Health @ Home: Free mental health workbooks to address a variety of mental illnesses.
MentalHealthatHome.org/2018/06/14/mental-health-workbooks/
Therapist Aid: Online Therapy Tools for Mental Health Professionals - Worksheets, interactive tools, videos, and articles.
TherapistAid.com/
Children’s Mental Health Matters: Maryland Public Awareness Campaign Resource Library
ChildrensMentalHealthMatters.org/resources/downloads/
RAINN Sexual Assault Hotline:
1 (800) 656-4673
National Helpline for Substance Use:
1 (844) 289-0879
Substance Abuse and Mental Health Services Administration National Helpline:
1 (800) 662-HELP or TTY 1 (800) 487-4889
American Academy of Child and Adolescent Psychiatry: Pediatric mental health updates and resources.
A AC AP. or g
National Federation of Families: Family support and advocacy.
FFCMH.org
Children’s Defense Fund: Child advocacy and research.
ChildrensDefense.org
Mental Health America: Mental health screening tests.
MHANational.org

Draft
School Nurse’s Mental Health Toolkit
Practical Strategies for Helping Students
2024 Edition
